Reductionism as a critical approach to understanding cancer
To understand highly complex biological systems, researchers typically apply a reductionist approach to their science. They focus their questions on smaller, more straightforward aspects of an entire system. For example, to understand how cancer works, a scientist might reduce a tumor down to a single cell and then probe the processes or molecular signals that go awry to cause uncontrolled growth. The knowledge of many cancer-relevant processes could then be integrated for a more complete understanding of the larger system of the tumor.
Reductionism underpins a great deal of what we know about cancer and has led to the discovery of many important cancer genes. For example, by studying viruses known to cause cancer, Harold Varmus and J. Michael Bishop, who shared the 1989 Nobel Prize for Physiology or Medicine, discovered that those viruses had acquired mutated forms of human and animal genes that caused aberrant cell growth and division. The realization that normal genes could transform into cancer-causing genes in viruses led to the discovery that a similar process takes place when cancer arises in human and animal cells.
Reductionist science has led to huge advances in knowledge and novel approaches to treatment, but it can be insufficient in getting us to a comprehensive understanding of how cancer works in the whole organism and can sometimes dampen our ability to discover and develop treatments that mitigate the most important features of a highly disrupted system.
Probing the “Science of the Patient” for deeper insights
To achieve the next generation of breakthroughs in cancer research, we may need to deliberately go beyond viewing a tumor within its local microenvironment to also viewing the characteristics of the host (i.e., the patient) along with the external influences of that host’s macroenvironment to gain richer insights regarding disease initiation, progression, and long-term consequences. Such focus on the “science of the patient” could address critical questions left unanswered by reductionist science.
For example, why do some people who are genetically predisposed to cancer never develop it? Researchers have identified families with genetic mutations that predispose them to cancer and have analyzed cancer patterns within these families. Yet some family members who carry these mutations manage to live cancer-free lives. We don’t know why — but the answers could be important to understanding the genetics or biology that leads to protection.
Another example of the “science of the patient” focus is cachexia, a wasting syndrome that, by some estimates, accounts for one-third of cancer deaths. Patients with cachexia dramatically lose muscular skeletal mass and body weight. They become extremely frail and weak, and some are not able to benefit from nourishment or tolerate their treatments. If we could mitigate cachexia, we could probably extend the lives of many cancer patients while getting them through treatment. Katy Ong, PhD, a postdoctoral fellow at UC Berkeley, whom we support in partnership with the Damon Runyon Cancer Research Foundation, is studying a new genetic tumor model in the fruit fly Drosophila melanogaster that simulates human disorders such as cachexia. Because fruit flies have a very short development cycle, it is easier to gain insights quickly and iterate on those findings to generate hypotheses that could be explored in humans.
We are also just beginning to understand the impact of stress in the pathophysiology of cancer. A recent study showed that an increase in certain stress hormones causes increased colonization of cancer cells in certain types of tumors and reduced survival. Neutrophils are a type of white blood cell that increase naturally in response to infections, injuries, and other types of stress. Research by Mikala Egeblad, PhD, at Cold Spring Harbor Laboratory, who received an ASPIRE award from us in 2019, has demonstrated that neutrophils play an important role in metastasis. Cancer cells hijack nearby neutrophils and force them to eject web-like structures called neutrophil extracellular traps (NETs), which may allow metastases to migrate to distant tissues. This research could lead to prevention strategies (e.g., the alleviation of stress) or therapeutics the mitigate the effects of NETs in patients.
Announcing our new Science of the Patient Grant in partnership with AACR
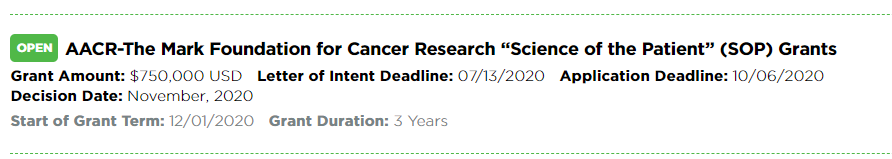
These are just some of the critical questions that studying the science of the patient could help answer. We at The Mark Foundation for Cancer Research are eager to explore more underserved areas of research like this. That is why we’ve just announced a partnership with the American Association for Cancer Research (AACR) on a new grant opportunity. Each AACR-Mark Foundation “Science of the Patient” Grant will provide $750,000 over three years to support highly innovative projects that will substantially advance our understanding of cancer initiation, progression, treatment, and survivorship. The LOI deadline is July 13.
Changing our vantage point for new cancer insights
Cancer is complex; cancer research is even more complex. Drilling down to the molecular level gets us certain kinds of information, but we also have to be willing to step back. A change in vantage point will lead us to different answers to different questions — and this may be what we need to truly transform our knowledge of the disease.



